e-Patients Blog
The blog of the Society for Participatory Medicine. Want to be a contributor?
Technology, Health Equity, and Participatory Medicine in the Care Management of Sickle Cell Patients
During my doctoral study in nursing practice a couple of years ago, I learned about a champion of nursing informatics, Dr. Nancy Staggers. Dr. Staggers assisted in developing the American Nursing Association’s Scopes and Standards of Practice. She also contributed to...
Driving Transformation: Change Management Strategies for Integrating Participatory Medicine in Healthcare
To implement successful change you must, unequivocally, understand the culture of the environment you are looking to change. Culture and change management are inextricably connected. Culture is a made up of a series of repeated, engrained, and expected behaviors and,...
The Challenge for Medicare Part D Patients: Inability to Utilize Pharmaceutical Programs to Reduce Medication Costs
Medicare Part D patients frequently aren’t allowed to take advantage of pharma pricing offers that reduce medication costs. This can leave patients unable to carry out the agreed treatment plan, which can harm their health outcomes.
Shared Decision-making: Becoming a Better Advocate for your Healthcare
I have a confession to make: I’m not always an effective advocate for my own care. It’s probably helpful for me to put this into context. I have been working in and around healthcare organizations for more than 25 years. I’m a researcher by trade, and worked with...
2024 SPM Update from Board Chair Mary Hennings
Our goal for the Society for Participatory Medicine in 2023 was to expand awareness of participatory medicine ([PM)] and SPM post-Covid and build new insights into the value of PM. We developed two curriculum modules, one on participatory medicine and the other on...
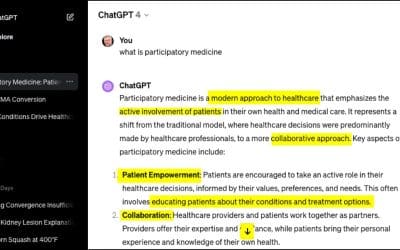
Hey ChatGPT, what’s Participatory Medicine?
I'm working on lots of things about generative AI in healthcare, because among other things, "GenAI" is incredibly empowering and liberating for e-patients. For kicks I decided to ask GPT-4 what it thinks participatory medicine is. Here's its answer. Couldn't have...
Uncle Sam Wants You! FDA’s new Digital Health Advisory Committee needs an e-patient voice!
As the World War I recruiting posters put it, “Uncle Sam Wants You!” In this case, though, it’s not the U.S. Army, but the U.S. Food and Drug Administration. The FDA, whose regulations touch 25 cents of every dollar spent by U.S. consumers, is launching a Digital...
A patient asks ChatGPT: cardio exercises after hip replacement?
Be cautious, be wise: AI tools like ChatGPT sometimes makes things up! Would you want a doctor who does that?? You can use AI to gather information and probe deeply for more details. But check your facts before you act. See tips at end of post. The world is still...
How to be an empowered patient, for seniors … outlined by GPT-4
Since our beginning in 2009 a big part of the vision for our Society has been to spread the word. Toward that end, this month I'm doing a talk at the Massachusetts Council on Aging annual conference, to launch a new topic I'll be using in local community...
ChatGPT summarized my OpenNotes. It’s so much more usable!
I had an idea last week and just tried it. ChatGPT is awesome at summarizing things, but could it handle medical notes? They're complicated. It worked! I took the visit notes from my last doctor appointment (the whole big, long, detailed thing) and asked...
A Surprising Collaboration Gives Trauma Patients a Second Chance
Emergency medicine has always been a collaborative practice, where teamwork and communication are paramount as first responders, nurses and physicians work together knowing that every second counts. While much has been written about collaboration during the clinical...
Moments that Matter: in-between routine care to emergency medicine
From shared-decision making, patient-centered care and value-based care to common technology innovations, healthcare players often describe how we aspire healthcare to be in concepts, buzzwords, branding and what has become common lexicon mentioned in conversations...