 Matthew S. Katz, MD, is the Medical Director of Radiation Oncology at Lowell General Hospital and a lifetime member of S4PM. He is former Chair of Communications Committee for the American Society for Radiation Oncology (ASTRO) and external advisor for Mayo Clinic’s Center for Social Media. He is co-moderator of the #radonc journal club and serves on committees for the American Society of Clinical Oncology and Massachusetts Medical Society. His main areas of interest are cancer care, patient education and health empowerment.
Matthew S. Katz, MD, is the Medical Director of Radiation Oncology at Lowell General Hospital and a lifetime member of S4PM. He is former Chair of Communications Committee for the American Society for Radiation Oncology (ASTRO) and external advisor for Mayo Clinic’s Center for Social Media. He is co-moderator of the #radonc journal club and serves on committees for the American Society of Clinical Oncology and Massachusetts Medical Society. His main areas of interest are cancer care, patient education and health empowerment.
E-Patients Deserve E-Doctors: Addressing the Needs of Both to Make Health Care Better for Everyone
Everyone deserves a chance to be healthy. Physicians, of course, focus on helping patients. Unfortunately, I often see patients’ frustrations with the health care system itself directed toward doctors.
Doctors are under increasing pressures on multiple fronts. Yes, we’re imperfect, but making physicians the primary focus of patient anger will not solve problems we all face as humans who will, at some point, need health care. (Note: I’m using doctors as an example for this piece, but my observations apply to all health care professionals.)
Patients need doctors. Doctors need patients. Let’s find a way to value both.
Patients deserve to be empowered
Health is more than not being ill. The World Health Organization definition puts the full range of patients’ needs first: “Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.”
How can patients achieve the health they deserve? Only if they’re empowered. The “e” in e-patient can mean many things, but if health is a basic human right, then empowerment is the only “e” that secures that right.
Being empowered means being able to meet certain fundamental needs, ones that need to be in place before we can make accurate, informed decisions about health. Here’s what we need for empowerment:
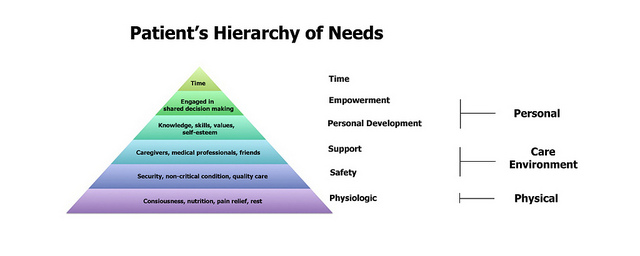 Image credit: Matthew S. Katz, MD
Image credit: Matthew S. Katz, MD
Autonomy is not absolute
Empowerment isn’t the same as autonomy. True autonomy is the ability to make an independent, free choice. Sometimes we don’t have the luxury of time; pain may color our perspective. Loved ones often can have strong influences upon our decisions. Humans are relational by nature, not truly independent.
Sometimes we disagree with health care professionals. Even when doctors or nurses want to help, their experience or ethical concerns may prevent them from giving us what we want or need. Patients are inherently vulnerable.
In addition, while more people may currently be involved with shared decision-making or perhaps even lead the process, not all patients want complete autonomy. Patient decision-making preferences may vary based upon many factors. It’s not reasonable to insist that patients lead decision-making if they want to receive guidance or direction from their physicians.
Patients deserve access, dignity, and a chance to be involved in decision-making, but that doesn’t automatically lead to satisfaction. In our desire for control, some of our choices may actually hurt us. Rather than being angry at doctors and taking our frustrations out on them, I suggest we recognize and explore common ground that may help patients and doctors alike.
Doctors are patients too
When we’re sick, we understand that others who suffer and need help will rightfully compete for doctors’ attention. What we often fail to remember is that those helping us may also struggle with health issues.
While data suggest doctors are becoming better than the general population about their health when it comes to smoking and obesity, physicians have higher rates of burnout and suicide. Multiple surveys show many medical students and doctors may have suicidal thoughts, with one study estimating that up to 24% of doctors have thought about taking their own life at some point in time.
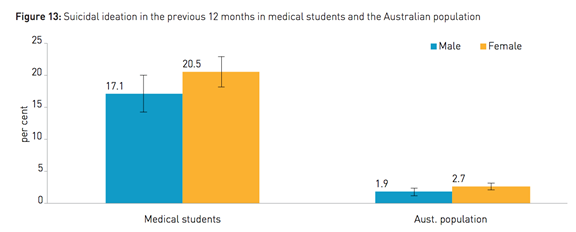
Source: beyondblue.org
Doctors haven’t made it easier on themselves. Excessively high expectations of a different era and a tendency to internalize stresses rather than seek help may lead to burnout, hopelessness, and self-harm. Access to medication also makes substance abuse a particular problem in some specialties.
Multiple factors contribute to physician burnout, depression, and impairment. We can’t solve or eliminate them all, but e-patients should want doctors to be healthy and well. Healthy doctors are more accessible, better listeners, and more able to dedicate time to patients. As a small subset of patients, doctors deserve mental and physical health to ensure they can be there for us when we need them.
So what do doctors need for empowerment?
Doctors also have a hierarchy of needs
Healers need to be healthy first—just like patients. Then, they need the right personal characteristics, training and support to be better able to do their job—helping patients.

Image credit: Matthew S. Katz, MD
With health and virtuous characteristics as the foundation of success, doctors can earn the right to the trust of patients and their caregivers as well as society at large. This model affirms the patient-doctor relationship and aligns patients and doctors.
Making it better for everyone
We are all dissatisfied with an unhealthy health care system in a rapidly changing world. Empowering patients and doctors ensures they can work together. New technologies and tests are not solutions; they’re just tools. If patients and doctors don’t stand up for themselves, other stakeholders (e.g., hospitals, insurers, industry) may unwittingly make things worse.
Thoughtful and vocal patients, caregivers and doctors should stand together. Even when we disagree, we can respect our differences while working toward solutions, both in clinic and for the health care system.
We both have a lot to bring to the table. Empowered patients are better able to collaborate. Empowered doctors are more able to adapt to each patient’s needs and communicate well to build trust. We need each other. And if we support each other, the entire health care system will be the better for it.
Note: Originally published on Mayo Clinic Social Media Health Network, 2014; updated for ASCOconnection.org on June 5, 2015; updated for SPM’s blog e-patients.net on June 16, 2015






Recent Comments