e-Patients Blog
The blog of the Society for Participatory Medicine. Want to be a contributor?
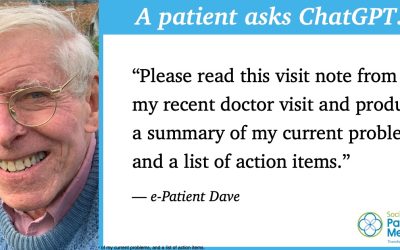
ChatGPT summarized my OpenNotes. It’s so much more usable!
I had an idea last week and just tried it. ChatGPT is awesome at summarizing things, but could it handle medical notes? They're complicated. It worked! I took the visit notes from my last doctor appointment (the whole big, long, detailed thing) and asked...
What My Second Lease on Life Taught Me about the Power of Human Connection
I was born with a congenital heart defect called bicuspid aortic stenosis with regurgitation. When I was 12 years old I was told I needed immediate open-heart surgery. As the anxiety, depression and sheer terror set in, my family tried to distract me by taking me on...
Building for Success: How Good Clinicians Can Empower Patients
Editor’s note: Ibrahim Rashid contracted Long COVID more than two years ago. The experience is propelling his patient advocacy and entrepreneurship, as co-founder of the digital health company Strong Haulers. In this excerpt from his new book, Strong Hauler: Learning...
How Trust Fuels Equitable Health Outcomes
At the Society for Participatory Medicine, we recognize trust and respect as a two-way relational dynamic essential to our mission to transform the culture of healthcare relationships so people can live their best lives (see our Participatory Medicine manifesto). And...
A Surprising Collaboration Gives Trauma Patients a Second Chance
Emergency medicine has always been a collaborative practice, where teamwork and communication are paramount as first responders, nurses and physicians work together knowing that every second counts. While much has been written about collaboration during the clinical...
Team Building In The Wake of the COVID-19 Pandemic
Editor’s note: In her new book, Communicating Through a Pandemic: A Chronicle of Experiences, Lessons Learned, and a Vision for the Future, Amelia Burke-Garcia, PhD, MA explores the many and varied roles that communication has played over the course of this pandemic,...
Update: How empathy, education, communication and the PAST Model transformed Sickle Cell patient care
Editor’s note: The following column by Society for Participatory Medicine board member Brenda Merriweather originally appeared in this space in December 2021. We are excerpting from that column in recognition of “Advancing Health Equity Through Participatory...
The Power of the Prescription Pad
At some point in our lives, we’ll be handed a little sheet of paper from our physician that has scribbled on it the medication we need, how much of it, and how often we should take it. These little slips of paper are power. They tell us that in order to get better, we...
Moments that Matter: in-between routine care to emergency medicine
From shared-decision making, patient-centered care and value-based care to common technology innovations, healthcare players often describe how we aspire healthcare to be in concepts, buzzwords, branding and what has become common lexicon mentioned in conversations...
BMJ publishes obituary of “Mighty Casey” Quinlan: Outspoken patient activist
The BMJ has published an obituary of lifetime SPM member "Mighty Casey" Quinlan. We (co-authors Jan Oldenburg and I) are thrilled that the editors, particularly obituaries editor Birte Twistleman, gave full voice to everything Casey. May her memory be a guiding light...
Through the Maze: A New Model for Equitable Health Data Exchange
My brother Jacob was born with a chronic neurological condition that caused him permanent physical and mental disabilities. As the only other child in a single parent family, I was often with Jacob during his frequent hospital stays and doctor visits. It is through...
A Reminder of How To Care Through Self-Reflection
After 28 years of nursing I could potentially consider myself an expert in the field. But this perception couldn’t be further from the truth. I still come home from a shift and often wonder and hope that I brought comfort to at least one patient. Did I do enough?...